Patients with two or more chronic conditions represent “64% of all clinician visits, 70% of all inpatient stays, 83% of all prescriptions, 71% of all healthcare spending, and 93% of Medicare spending.” (AHRQ MCC).
The prevalence of chronic conditions is increasing, costs are accelerating, and we have a staffing crisis.
The costliest patient groups are easy to identify through risk stratification, the hard thing is to engage and manage them effectively with technology. Patients with multiple chronic conditions are typically older citizens and/or people from ethnic minorities or those living in deprived communities.
We have proven with over 200,000 patient successes that ‘simple’ SMS-text powered by intelligent algorithms can reach all patient groups and deliver astonishing outcomes. We also automate care and save very significant clinical time and money. See below About Florence.
Common Chronic Conditions
The most common chronic conditions are, in alphabetical order, asthma, arthritis, depression, diabetes, and heart disease (AHRQ Vision).
Of the population 50 years and older, the number with at least one chronic disease is estimated to increase by 99.5% from 72 million in 2020 to 143 million by 2050; at the same time, those with multimorbidity are projected to increase 91.16% (Ansah and Chiu 2022).
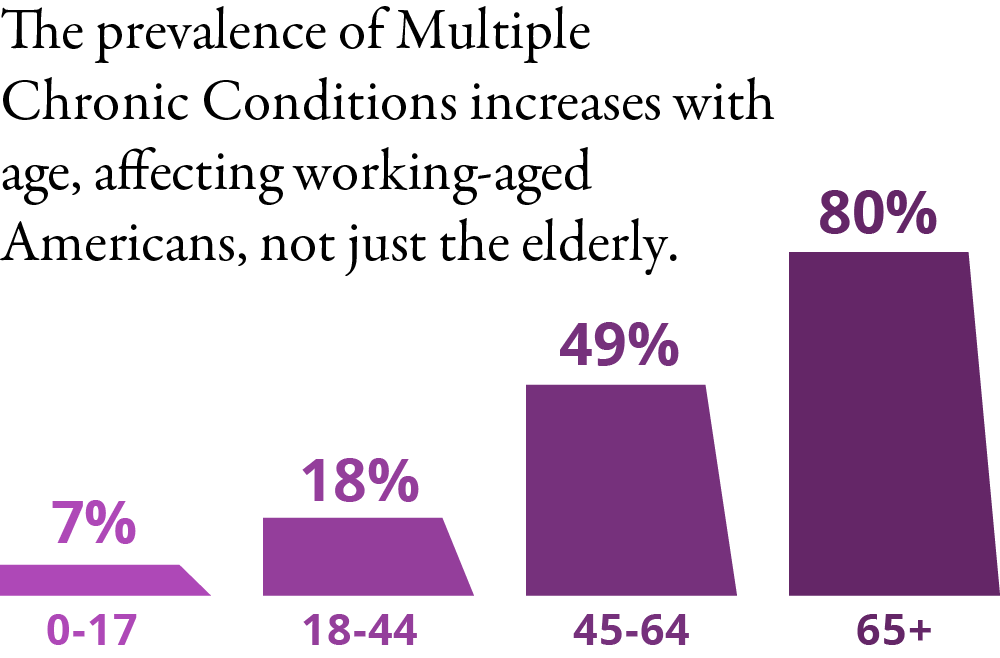
The prevalence of multiple chronic conditions increases with age, with 49% of the population aged 45-64 living with MCC and a whopping 80% of those over 65 of age (AHRQ Vision).
Though the main clusters of chronic conditions are fairly well known, see diagram below based on Ward and Schiller 2013, the key challenge is developing effective programs to manage these patients.
Most prevalent clusters of conditions in patients with two or three chronic conditions:
| Men | Women | |
| Dyad (=2 conditions) | Diabetes / Hypertension | Diabetes/Hypertension Except aged 18-44: Arthritis / Asthma |
| Triad (=3 conditions) | Arthritis / Diabetes / Hyper/tension | Arthritis / Diabetes / Hypertension Except aged 18-44: Arthritis / Asthma / COPD |
At Generated Health we believe the solution is enabling and driving behavior change, including self-management. Read here about the framework we use for our Intelligent Health Messaging: HERE
Value-Based Care… finally momentum
The traditional fee for service-model is broadly recognized as broken. With the acceleration of chronic conditions, and particularly multiple chronic conditions, there is no other option than to deliver more patient-centered care within a VBC-framework.
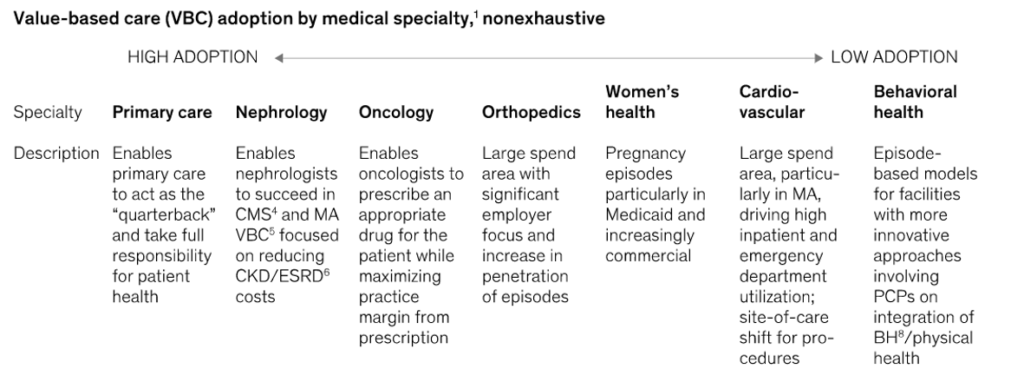
McKinsey calculates that in a high-quality VBC-model, the savings are as much as 20% for high-touch primary care groups taking full capitated risk on Medicare Advantage members (McKinsey VBC 2022). Accordingly, they expect the most rapid VBC adoption in primary care and nephrology with the slowest adoption in behavior health, as set out below.
It is clear that investors have also woken up to the fact that VBC is now (finally many would say) gaining traction. McKinsey suggests that from 2019 to 2021 the investment in private value-based care companies increased 4x while investment in hospital infrastructure remained relatively flat.
Kaiser Permanente supports the idea of adoption in primary care. When analyzing the top 5% of the population driving ca 50% of cost, they believe the most effective strategy is ‘leveraged primary care’ (HRB 2020). Kaiser Permanente notes that within the top 5% group, ca two-thirds relate to chronic conditions and one-third acute events. The most interesting observation is that the chronic condition cohort is very fluid (so people move in and out of the top 5% at pace) – therefore the biggest return comes from casting a wider net and manage ‘raising risk’ from people well below the 5% group.
VBC momentum – where? Medicare Advantage, with 35% of payments through alternative models (APMs) and traditional Medicare (24% through APMs) are leading the way according to the latest HCPLAN report (LAN 2022) and Medicare, which covers 1 in 4 US citizens, is seen as the immediate growth area for VBC adoption.
About Florence: SMS-Text Patient Management & Care Automation
We use ‘simple’ SMS – to engage patients and drive self-management – powered by intelligent algorithms. We save healthcare teams time – 60% fewer visits / 70% fewer hospital admissions – while delivering incredible outcomes.
Our approach works particularly well with patients with multiple chronic conditions. See video of how Stuart is managing both hypertension and diabetes with the support of Florence.
Over 200,000 patients in UK and Australia are successfully managed by Florence – examples of benefits include:
- 109 hours saved per patient in enteral feeding and blood pressure.
- 75% reduction in hospital visits for patients with diabetes
- 50% improvement in symptoms of depression
- $35,000 saved per patient w COPD by reducing hospital admissions by over 60%
Contact us to schedule a call with one of our experts or see a demo.
REFERENCES
- AHRQ Vision: https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/multichronic/mcc.html
- Ansah and Chiu 2022: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9881650/#:~:text=Of%20the%20population%2050%20years,to%2014.968%20million%20in%202050
- Ward and Schiller 2013: https://www.cdc.gov/pcd/issues/2013/12_0203.htm#:~:text=As%20for%20the%20most%20prevalent,and%20ever%20having%20had%20hypertension
- McKinsey VBC 2022: https://www.mckinsey.com/industries/healthcare/our-insights/investing-in-the-new-era-of-value-based-care
- LAN 2022: http://hcp-lan.org/workproducts/apm-methodology-2022.pdf
- HBR 2020 https://hbr.org/2020/01/managing-the-most-expensive-patients