‘The patient is the largest and least utilized resource in healthcare’ to quote Warner Slack, the visionary physician. Unhealthy behaviors account for nearly 40% of premature deaths and substantial morbidity in the US (1) and, for most chronic conditions, modest lifestyle modifications can be impactful.
Given the impact, you would think clinicians would be focused on behavior change. The sad reality is that patients do listen to clinicians; it is just that clinicians are not engaging. Only 10–20% of smokers report being told to quit smoking by their clinician; less than 20% of obese patients report being told by their clinician they are overweight (2).
If humans can’t (due to time) or want (because it’s uncomfortable) deliver systematic, frequent engagement and coaching to drive behavior change, then we must look to automation.
That is why Florence, our digital nurse, delivers Automated Clinical Conversations via Text powered by Evidence-Based AI. It is simple and scalable. Text reaches everyone, and it’s remarkably effective. www.generatedhealth.com has proven success across over 200,000 patients in English, Spanish, and Arabic. Validated studies include 64% less nurse-time while improving A1c by one point, 70% reduction in emergency admissions for COPD patients, and a pharmacist team reducing clinician work by 75% and admin work 10-fold in hypertension medication titration. More details are at the bottom of this blog.
Chronic Conditions: Behavior Change or Death (and Substantial Costs)
Chronic disease, including mental health, is now totaling 90% of all healthcare costs in the US (3), and the prevalence is increasing. The number of adults, aged 50 and over, with at least one chronic condition, is estimated to increase 99.5% from 72 million in 2020 to 143 million by 2050; a 91% increase to 15 million is expected for those with multimorbidity (4). It is no better in young adults, with 54% of 18–34-year-olds reporting at least one chronic condition and 22% reporting having more than one, with the highest prevalences in obesity (25%) depression (21%) and high blood pressure (11%) (5).
Evidence shows that positive lifestyle changes such as more exercise, weight loss and smoking cessation have positive effects on health outcomes – for example a small cohort of diabetic patients using Florence lost an average 16kg with an associated 33% reduction in HbA1c levels (6). Engaging patients in health behavior change has been clearly demonstrated to slow down chronic conditions. A 10-mmHg reduction in blood pressure reduces the risk of heart attacks and strokes by 20% (7) and every 1 mmol/L reduction in cholesterol (LDL-C) levels reduces the risk of major vascular events after one year by 22% (8)
Behavior Change: Science Easy, Implementation Hard
The research around human behavior has exploded in the last decade and new theories and frameworks are emerging all the time. Despite this, at a practical, scalable level, ‘everyone’ agrees that optimal care for chronic disease should include activities to support patients in self-management, including goal setting and counseling patients to adopt healthy behaviors and to integrate skills at managing their disease on a day-to-day basis.
There are a number of frameworks or tools for clinicians to choose from, many that both overlap and are complementary, including:
- Five Rs for patients that are not ready to make a health behavior change clinicians are recommended to: (i) discuss the Relevance of the change for the patient (e.g. smoking may be contributing to your getting so many colds and missing work so often), (ii) discuss the Risks of continuing the unhealthy behavior, (iii) discuss the Rewards of adopting a healthy behavior, (iv) identify Roadblocks to changing the behavior, and (v) Repetition of the personalized five Rs message at each visit (9).
- Five As is a framework that can help guide clinician actions to health behavior change: (i) Ask every patient about health behaviors, (ii) Advise patients with an unhealthy behavior in a clear, strong, and personalized manner to modify the behavior, (iii) Assess the patient’s willingness to change the health behavior (sometimes referred to as seeking Agreement on the patient’s willingness to change the health behavior), (iv) Assist the patient in modifying the health behavior, and (v) Arrange for follow-up.
- Motivational Interviewing seeks to leverage a patient’s values and goals to initiate and maintain behavior change. Motivational Interviewing is a 100% patient-centered, directive method for enhancing intrinsic motivation. Key is ensuring the patient has a knowledge of how the behavior change relates to their personal goals and sense of self in the context of family and community, and their other values and roles.
The challenge with all of these? It requires time and personalization. It also requires follow-ups and repetition. All hard in a busy day.
Clinicians: So Much to Do….and it’s Hard to Talk About ‘Behaviors’
Although there is significant evidence of the ability of clinicians to influence patients to change unhealthy behaviors, it is unfortunately not happening at scale.
Studies have shown that few patients report being asked regularly about their health behaviors; fewer than 20% of obese patients are being told to lose weight, fewer than 20% of smokers report being told to quit smoking by their clinicians; and only 2–5% of patients in need of intensive diet, exercise, and weight loss counseling receive assistance (10).
Despite accounting for nearly 40% of premature deaths and substantial morbidity, why are clinicians ‘not doing it’?
The key driver is time: short-staffed healthcare teams are exhausted, jumping from crisis to crisis. It is human to deal with what is important and right in front of us; it is hard to focus on important activities that are not deemed urgent. More on this in our article on Staff Shortages and Clinical Inertia.
Healthcare workers are increasingly experiencing burn-out by ever-increasing demand and a sense that that they are not ‘doing enough’ for patients. One qualitative study on physicians’ perspectives on caring for patients with chronic pain, found that HCPs internalized feelings of failure, guilt and discontent (11). Behavior change coaching requires mental bandwidth and is hard to do when clinicians themselves are balancing on the edge.
Addressing behavior change such as smoking, weight loss or stress can be seen as an uncomfortable intrusion into a patient’s private space and is potentially made harder by fear of insensitive treatment of minorities or vulnerable people. We repeatedly hear that healthcare professionals feel uneasy when questioning patients on social determinants of health (SDOH).
Automated Clinical Conversations via Text: Delivers Behavior Change
Since our platform Florence was first conceived, the focus was on simple, scalable text ‘conversations’ designed to empower behavior change and drive self-management.
Based on over 25 million conversations via text, and over 200,000 patient successes it is clear: Everyone wins. Patients make sustained behavior changes leading to better health and clinical outcomes and substantial savings of staff time:
- Diabetes: 64% less time spent, A1c reduced by 1 point
- Heart failure: Hospital admissions reduced by over 65%
- Hypertension: 50% fewer appointments, sustained improvements
- COPD: 70% reduction in emergency admissions
Florence is now hard at work 24/7 in England, Scotland & Wales, Australia, and across the US, supporting patients in their management of chronic conditions, and in pre and post operative care (periop).
A ‘personable robot that holds patients to account’, says Lindsey, a nurse practitioner in Newport, Maine, that will ‘check in with you, see how you are feeling, that you are taking your meds or whether you need a dose change.’
‘A regular doctor, that is why I like it,’ according to one patient. https://generatedhealth.com/us/video/diabetes-success-with-flo
Behavior Change: How Florence Actually Works?
Patients typically describe Florence as someone who is both ‘looking after me and holding me accountable’. She works just like a competent and compassionate nurse – with one exception – she is working 24/7 and she is always following the SOC or protocol.
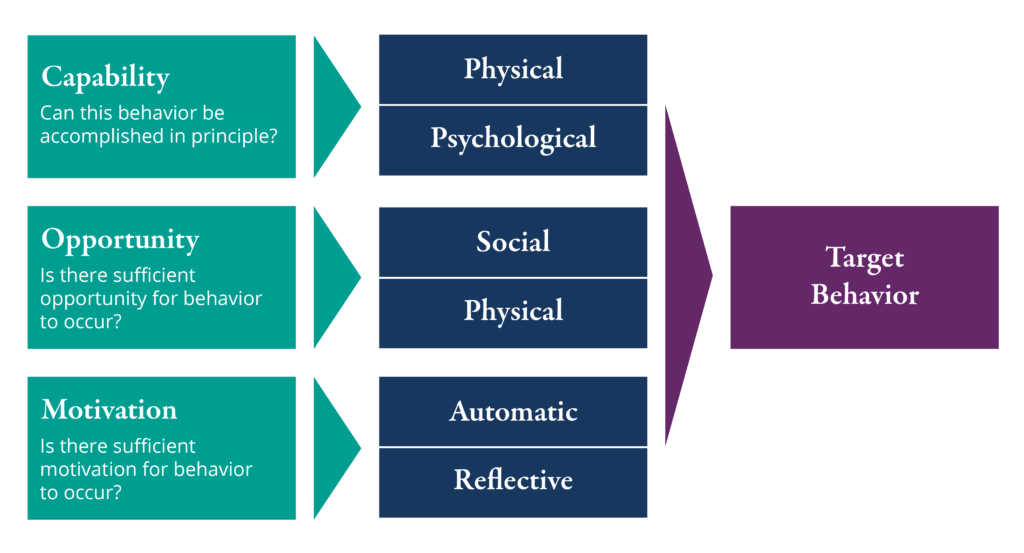
Florence has been developed with the input and support from over 500 clinicians. The underpinning has been the Behavior Change Wheel and the simpler COM-B model below.
Florence is not shy about asking about healthy or unhealthy behaviors (smoking, drinking, weight, stress, etc.) and she will work with patients to develop simple achievable plans based on motivational interviewing.
Her biggest strength is persistence; Florence will engage with patients two to three times per day if necessary and sometimes just once a week, requesting readings, providing educational material and crucially providing feedback on progress.
We are on a mission to create 1 million nurses, powered by AI, that empower sustained behavior change and drive patient self-management.
Contact us for further details www.generatedhealth.com
US: EBender@generatedhealth.com
UK: John.Griffiths@generatedhealth.com
Aus: Kylie.Dentith@generatedhealth.com
References
1. (Mokdad, et al.,2004)
2. (Leverence, et al., 2007) (Rothemich, et al., 2008)
3. Centers for Disease Control & Prevention
4. (Ansah & Chiu, 2022)
5. (Watson, et al., 2022)
6. Diabetes, Flo improves efficacy of best practice care
7. (Kearney & Freeman, 2016)
8. (Sabatine, et al., 2018)
9. (Glanz, et al., 2008) (Glanz & Rimmer, 2005)
10. (Leverence, et al., 2007) (Rothemich, et al., 2008)
11. (Matthias, et al., 2010)