Mental Health
With the World Health Organisation citing adherence to therapies as a primary determinant of the effectiveness of treatment1 South Eastern Melbourne Primary Health Network (SEMPHN) clinicians have been harnessing Nellie’s unique ability to motivate and engage patients towards positive behaviour change.
Jennifer, age 50 (not real age or name) living with chronic mental health challenges and associated physical health co-morbidities kindly wrote to the SEMPHN team to share the impact of her supportive intervention with Nellie. Jennifer’s clinician, Dr Wild, had targeted Nellie to support the specific medication adherence challenges demonstrated by the patient.
Jennifer’s letter described the impact that this made to her physical and mental health and how it enabled her to adopt behaviours to sustain her medication adherence beyond her interventional support from Nellie. The improvements were significant and enabled her to commence cognitive behavioural therapy (CBT) and interpersonal therapy (ITP) programmes.
Jennifer’s letter explained that due to her existing medical condition, her clinician had recognised that she was often going to bed forgetting to take her medication despite having a tablet box filled each week by her daughter. Unfortunately, the patient’s suboptimal medication adherence was exacerbating her memory problems, and as a result Nellie was introduced to Jennifer’s daily routine to prompt her before bedtime to provide a real time intervention aimed at improving her adherence and subsequently reducing the physical and mental impact of previous non compliance.
Jennifer’s clinician personalised Nellie’s interactive messages and agreed with her the best time for Nellie to remind her during her evening routine. Nellie would also ask Jennifer to confirm that she had taken her medication, which provided reassurance for her clinician that Jennifer’s adherence was improving, and importantly allowed an opportunity for the clinician to take further action should they be notified by Nellie that medication had been missed.
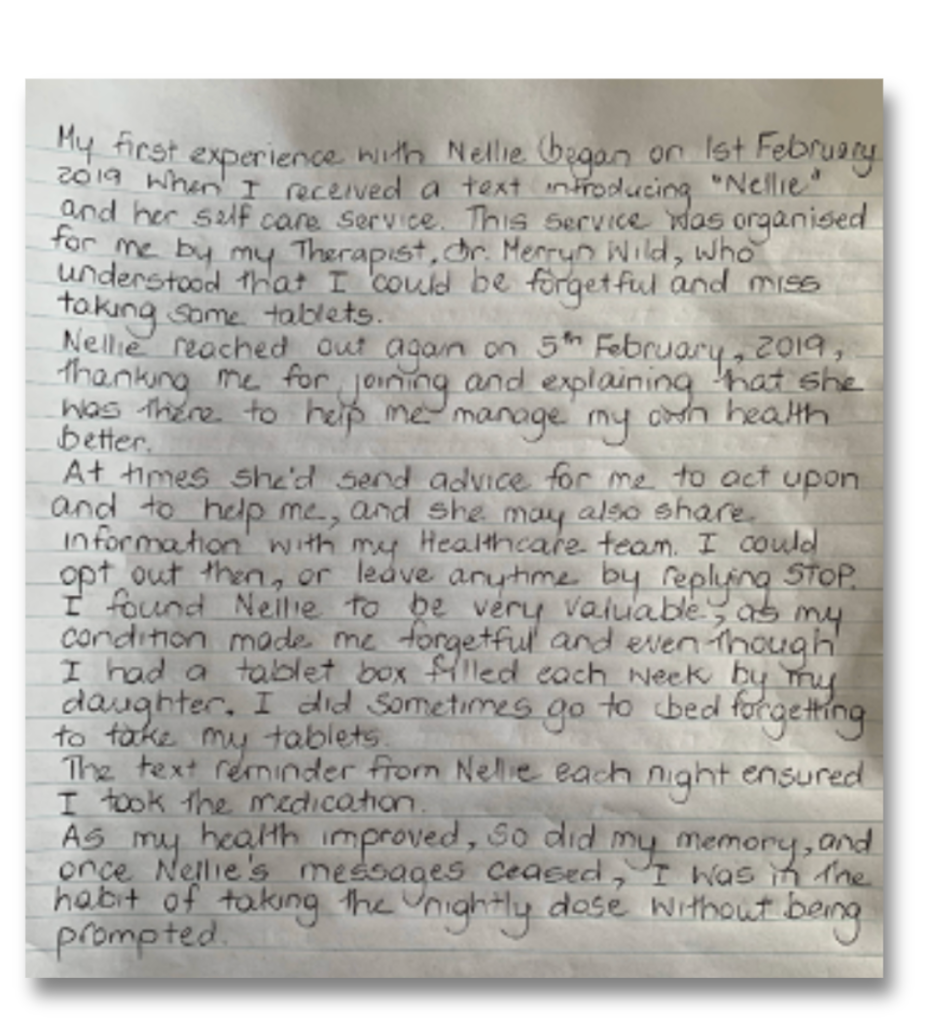
With Nellie’s gentle prompts, Jennifer started to take her medication as prescribed, her memory problems began to reduce and her physical and mental health improved; by the time her programme with Nellie had ended she was comfortably in the habit of taking her medication independently as prescribed each evening. Jennifer also explained that as her memory problems had now improved, she had now begun initiating the filling of her tablet box whenever her daughter had forgotten, demonstrating positive behaviour change and a shift to sustainable independence around her medication.
“As my health improved, so did my memory, and once Nellie’s messages ceased, I was in the habit of taking the nightly dose without being prompted”
Interestingly, Nellie became such a part of the family that when Nellie’s programme of interactions ended, there was lots of positive speculation about why? Jennifer was able to tell her family that her confidence had improved considerably and now confident enough to manage her medication without Nellie’s support.
Jennifer remains close to being 100% compliant with her medication which far exceeds the average rate of compliance for most patients and is able to increase her independence around managing her condition.
To find out more about Nellie in Australia, click here