Healthcare Inequalities

Supporting the approach to reduce health inequalities with the NHS
Healthcare inequalities are avoidable, unfair differences between a person’s health status and group factors. Some examples are:
- Life expectancy
- Access to available services
- Smoking rates
- Quality of housing
- Income
- Geography
- Specifics characteristics
These factors, and many more, can also be interlinked. For example, unemployment may lead to poorer living conditions, less access to fresh food and recreation facilities. Resulting in some communities and groups to experience poorer health than the general population, and experience challenges in accessing the appropriate care. Yet, health inequities are often preventable.
The pandemic has played a big part in highlighting healthcare inequalities but it has also been a catalyst to widening the impact even further; COVID restrictions having a negative impact on disabled people vs non-disabled, mental health, waiting lists crisis and financial insecurity.
NHS Initiatives to reduce healthcare inequalities - Core20PLUS5
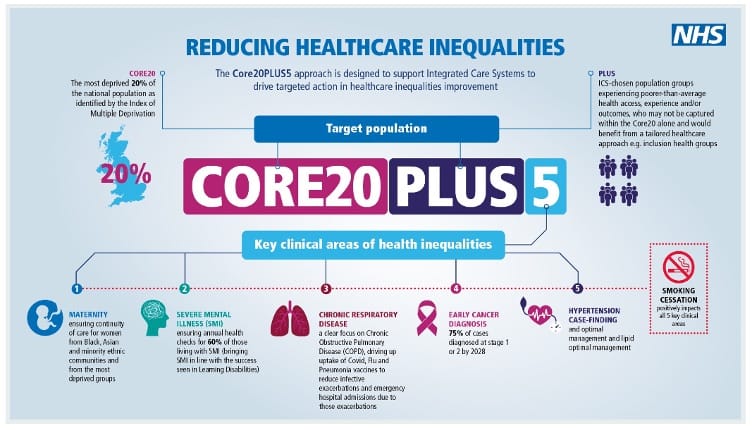
The NHS have a super-matrix approach across all NHS England programmes to drive improvements in healthcare inequalities by introducing such frameworks as Core20PLUS5 and the Health Inequalities Improvement dashboard. All with the same goal, reduce health inequalities in healthcare.
The NHS Core20PLUS5 framework looks at the deprived 20% of the national population plus population groups such as ethnic minority communities, inclusion health groups such as drug and alcohol dependence, Gypsy, Roma and traveller communities and people with learning disability, to name but a few.
It then sets out five clinical areas of focus:
- Maternity
- Servere Mental Illness
- Chronic Respiratory Disease
- Early Cancer Diagnosis
- Hypertension
To find out more, visit the NHS website – Core20PLUS5
How Florence Intelligent Health Messaging can support your Core20PLUS5 framework?
Florence provides intelligently enabled care that supports the Core20PLUS5 five clinical areas as well as the whole healthcare ecosystem.
In Acute care, extending the reach of hospital clinicians to improve patients’ motivation and capability to self-care, at pre-admission, post discharge and between outpatient clinic visits.
In Community care, supporting community practitioners to improve patient engagement with their health and track emerging symptoms to optimise clinical time and release capacity to support these patients most in need.
In General Practice, supporting clinicians in general practice to deliver sustained improvements to clinical outcomes for patients with long-term conditions.
Florence is the most accessible way to engage your most deprived patients to increase access and outcomes across the NHS:
- Expectant mums are monitored for pregnancy induced hypertension and gestational diabetes. New mums are supported with breastfeeding.
- SMI Health checks can be conducted remotely, reducing impact on SMI patients and increasing efficiency for clinical teams
- Increase uptake of COVID, Flu and Pneumonia vaccines with prompts, nudges and reminders
- Find and manage hypertensive patients by inviting at risk groups to Measure BP remotely without increasing workload for clinicians or administrators.
Useful resources about healthcare inequalities
Yorkshire & Humber, and Wessex
Florence features within the Yorkshire & Humber and Wessex AHSN horizon scan under Hypertension, which identifies innovations within healthcare that they believe will be of value to health and care providers to address inequalities.
Florence and the Gypsy, Roma & Travellers
